240 million people affected worldwide 1 2
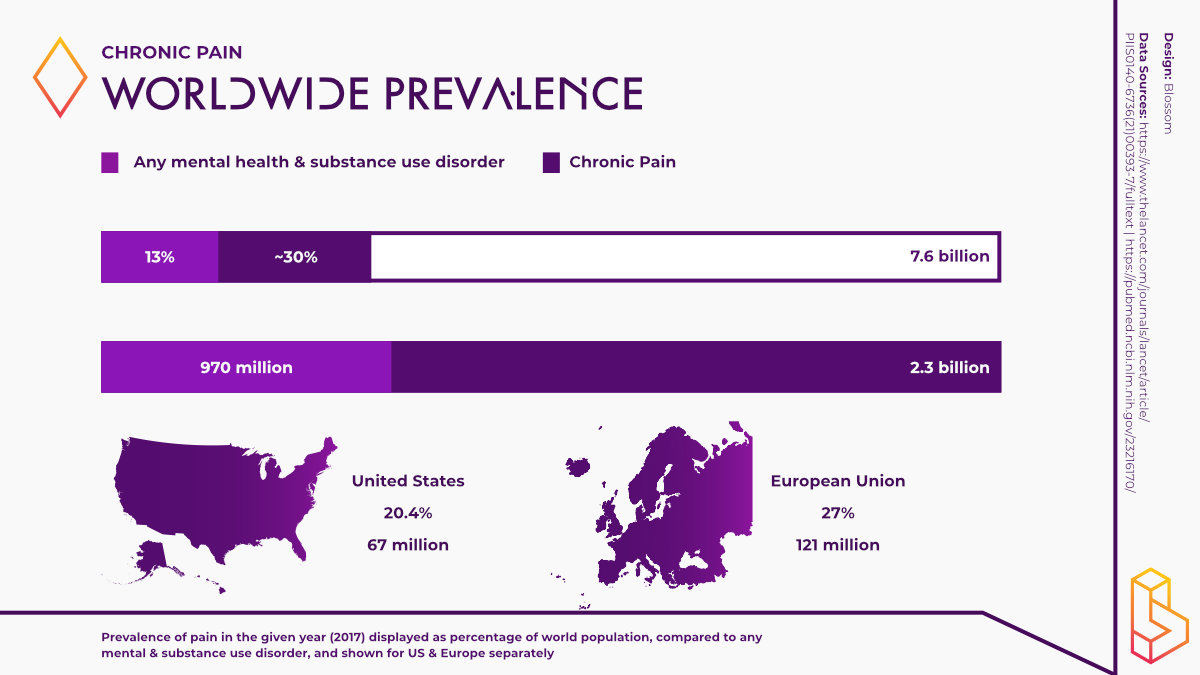
It is estimated that chronic pain affects at least 30% of the world’s population. The Global Burden of Disease Study 2016 reaffirmed the position of pain and pain-related disease as a leading cause of disability and the disease burden globally.
Current Treatments 1
Common techniques used to treat pain include; electrostimulation therapy, physical therapy, exercise, alternative therapies like acupuncture or various mind-body therapies. A range of prescription drugs exist to treat pain, the most infamous are known as opioid analgesics. This class of drugs includes morphine, codeine and oxycodone. Although opioids are effective in treating pain, when misused, these drugs can lead to addiction, overdose and even death
Psychedelic research currently is in Phase Ia
Few studies exist exploring the use of psychedelics to treat pain. A case study at UC San Diego found that psilocybin is safe and effective for treating phantom limb pain in the study's single participant. A trial is underway at University Hospital Basel to use LSD to treat Cluster Headaches.
Key Insights
- Roughly 30% of the world’s population lives with chronic pain. In high-income and high-middle-income countries, low back pain and migraine were the leading causes of YLDs (years lived with disability) in 2016.
- Psychedelic research in this area is in its early stages. Some successful case studies have taken place with psilocybin and ketamine. However, clinical trials are underway exploring the potential of substances like LSD, while DMT has also been proposed to be effective.
- Given the scarcity of research, a select few companies like PharmaTher and MindMed are exploring this avenue of psychedelic medicine. However, as we contend with the fallout of the opioid crisis, it is likely more companies will enter this space as more effective pain management tools are needed.
What is pain?
The International Association for the Study of Pain defines pain as “an unpleasant sensory and emotional experience associated with or resembling that associated with, actual or potential tissue damage” [1].
Pain has physical and emotional components that lead to unpleasant sensations ranging from mild, localised discomfort to agony [2].
Typically, pain is the body’s natural physiological response to noxious (harmful) stimuli. The pain signal relayed along the nervous system helps us protect a damaged body part while it heals and helps us avoid similar experiences in the future.
While the acute pain response generally subsides over time, pain may become chronic if the physiological response triggered by pain persists [3]. In this sense, acute pain usually comes on suddenly and is caused by something specific like a broken bone, burns or cuts.
Chronic pain usually lasts for longer than six months, persisting long after the injury or illness that caused the initial pain is healed. Chronic pain is linked to headaches, nerve pain, cancer, and fibromyalgia [4].
The personal and economic burden relating to chronic pain is enormous. According to some studies, it is estimated that more than 30% of the world’s population is affected by chronic pain [5].
The most recent Global Burden of Disease Study, the most comprehensive worldwide observational epidemiological study, reaffirmed the position of pain and pain-related disease as a leading cause of disability and the global disease burden [6]. The study found that low back pain and migraine were the leading causes of YLDs (years lived with disability) in high-income and high-middle-income countries [7].
Other common chronic pain conditions include recurrent tension-type headaches, neck pain and arthritis/joint pain. Living with chronic pain can severely impact a person’s ability to carry out normal day-to-day functions.
Diagnosis and Treatment
Pain is difficult to measure due to its multifaceted and subjective nature [8]. However, there is a range of tools at the disposal of medical professionals to aid in diagnosing pain.
These tools include CT scans, MRIs, bone scans or electromyograms (EMGs), to name a few. The American Chronic Pain Association developed the Quality of Life Scale for Pain (QLSP). The QLSP shows how pain affects one’s ability to work, socialise, exercise, and perform household tasks. The Visual Analog Scale is another widely used tool to measure pain. The Defence and Veterans Pain Rating Scale was developed to measure pain in the veteran population.
Given the complex nature of pain, a range of treatment options exists to help people better manage whatever pain they are experiencing. Patients experiencing pain may receive consultation from a physician who specialises in pain management, a physical rehabilitation specialist, or a psychiatrist to help people experiencing anxiety and depression due to their pain [9].
Common techniques used to treat pain include electrostimulation therapy (e-stim), physical therapy, exercise, and alternative therapies like acupuncture or mind-body therapies. A range of prescription drugs exists to treat pain, the most infamous of which is known as opioid analgesics.
This class of drugs includes morphine, codeine, and oxycodone. Although opioids effectively treat pain, when misused, these drugs can lead to addiction, overdose and even death [10].
We have become all too familiar with the so-called opioid overdose epidemic that is devastating the US and parts of Canada. In 2021, overdose deaths reached record levels in the US, surpassing 100.000. The majority of these overdoses were directly attributed to opioids [11].
Consequently, accidental drug overdose from opioids is now a leading cause of death in Americans under the age of 50 [12]. As the US grapples with the fallout of this crisis, researchers are turning to the potential of psychedelics as an alternative treatment and effective tool in pain management.
Psychedelics and Pain
Generally, psychedelics are considered physiologically safe and do not lead to addiction, making them a more practical approach to pain management.
The Psychedelics and Health Research Initiative (PHRI) was recently launched at University College San Diego (UCSD). This multidisciplinary initiative is researching the use of psychedelics to treat pain conditions, including cluster headaches, complex regional pain disorder, and phantom-limb pain.
A 2020 review by PHRI members Timothy Furnish, Joel Castellanos and Adam Halberstadt, experts in pain medicine, provides sustenance for the use of psychedelics to treat pain and a possible mechanism of action.
The researchers propose that the serotonin 2A (5-HT2A) receptor agonism properties of psychedelics may help modulate pain pathways in humans and that alterations in functional connectivity seen with psychedelics can reverse the changes in neural connections seen in chronic pain states [13].
A more recent review of the potential of psychedelics to help treat pain proposed similar mechanisms of action to that of Castellanos and colleagues. This review takes a deep dive into the neurophysiological mechanism underlying the use of psychedelics in pain management.
The review explores the potential neuro-restorative effects of psychedelics in pain-related states of consciousness, the anti-neuroinflammatory, and pro-immunomodulatory actions of psychedelics. Furthermore, the authors postulate that psychedelics could also help elucidate the mechanism of pain syndromes.
Psilocybin, LSD and Pain
A 2018 case study (n=1) conducted at UCSD successfully utilised psilocybin combined with mirror visual feedback (MVF) to treat phantom-limb pain. The researchers found that the psilocybin-MVF pairing demonstrated synergistic effects in eliminating acute and long-term phantom-limb pain (PLP) and decreased the recurrence of its episodes.
Psychedelics also hold promise for treating cluster headaches, a severely debilitating pain condition. Clusterbusters have been advocating for the use of psychedelics to treat cluster headaches since 2002. Based on the advocacy of Clusterbusters, the first psychedelic study at Harvard in over 40 years explored cluster headaches.
This qualitative interview study found that a single dose of psilocybin or LSD was often sufficient to terminate a cluster period. Sub-hallucinogenic doses were also often reported to be effective treatments.
An older Clusterbusters survey study (n=496) found that indolamine psychedelics like psilocybin and LSD are reportedly comparable to or even superior in efficacy against cluster headaches to conventional treatments. Again, sub-hallucinogenic doses of these substances were reportedly sufficient for this effect to occur.
Qualia Computing is another initiative at UCSD that has proposed using DMT and other tryptamines to treat cluster headaches.
A trial is also underway at University Hospital Basel, Switzerland, exploring the effects of LSD on cluster headaches. Furthermore, a recent study exploring the effects of microdosing LSD showed increased pain tolerance in participants.
In preparation for an upcoming clinical trial, researchers at Imperial College London conducted interviews (n=11) with people living with chronic pain to understand better how they self-medicate with psychedelics. Across different psychedelic substances, participants reported improved pain scores during and after psychedelic experiences.
A recent survey study (n=354) of people living with fibromyalgia assessed this cohort’s knowledge surrounding and use of serotonergic psychedelics. It was found that 29.9% of respondents reported past use of a psychedelic, while perceptions regarding benefits from use were generally neutral (59.4%) or positive (36.8%). Less than 3% reported that psychedelics negatively impacted their overall health or pain symptoms. Noteworthily, 11 out of 12 patients using psychedelics specifically to treat pain reported improvements in their symptoms.
Ketamine and Pain
Some trials and case studies have also explored ketamine to treat pain. A randomised, crossover, placebo-controlled, lab-based trial (n=22) tested the hypothesis that low dose ketamine blunts perceived pain and subsequent sympathetic and cardiovascular responses during an experimental noxious stimulus. The authors found that low dose ketamine (20 mg) administration attenuates perceived pain and pressor, but not muscle nerve activity response frequency, responses during a cold pressor test.
An observational pilot study (n=6) found that one of ketamine’s metabolites, (2R,6R)-hydroxynorketamine, could reduce pain with analgesic effects lasting up to one week in patients with refractory chronic migraines.
In a case study, a terminally ill cancer patient administered repeated low-dose ketamine infusions (<35mg/70kg) as an adjuvant pain control medication. The patient reported a sustained reduction in pain level and a reduction of total opioid usage in response to three consecutive ketamine infusions, which implicates its utility for improving the treatment of refractory pain within palliative care.
Psychedelic Industry and Pain
A select few companies are hoping to utilise the therapeutic potential of psychedelics to treat pain.
Toronto-based biotechnology company PharmaTher has focused on researching, developing, and commercialising novel uses, formulations, and delivery methods of psychedelics to treat mental illness, neurological, and pain disorders.
Earlier this year, PharmaTher partnered with MediSynergics to develop a patented ketamine formulation for treating pain.
MindMed recently announced the launch of Project Angie, a project dedicated to investigating the effects of LSD in a severe pain indication. The company hopes to begin a Phase IIa study in the near future following the submission of a pre-IND to the FDA.
Based in Santa Barbara, Bexson Biomedical is also focusing on treating pain, among other disorders, using ketamine. Currently, their lead project is a minimally invasive, wearable infusion that will deliver a proprietary formulation of ketamine. Bexson recently raised $4.8 million to support the company through pre-clinical and manufacturing scale-up for its proprietary ketamine formulation, BB106.
With the deaths attributable to opioids showing continuing to devastate the U.S., it is likely that more research, and more companies, will emerge that are dedicated to using psychedelics as viable therapy options for pain management.
References
1. Raja, S., Carr, D., Cohen, M., Finnerup, N., Flor, H., Gibson, S., . . . Ringkamp, M. (2020). The Revised IASP definition of pain: concepts, challenges, and compromises. Pain, 1976-1982. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7680716/
2. Davis, C. (2021). Medical Definition of Pain. MedicineNet. https://www.medicinenet.com/pain/definition.htm
3. Swift, A. (2018). Understanding the effect of pain and how the human body responds. Nursing Times, 22-26. https://www.nursingtimes.net/clinical-archive/pain-management/understanding-the-effect-of-pain-and-how-the-human-body-responds-26-02-2018/
4. Cleveland Clinic. (2020). Acute vs. Chronic Pain. Cleveland Clinic. https://my.clevelandclinic.org/health/articles/12051-acute-vs-chronic-pain
5. Cohen, S., Vase, L., & Hooten, W. (2021). Chronic pain: an update on burden, best practices, and new advances. The Lancet, 2082-2097. https://doi.org/10.1016/S0140-6736(21)00393-7
6. Mills, S., Nicolson, K., & Smith, B. (2019). Chronic pain: a review of its epidemiology and associated factors in population-based studies. British Journal of Anaesthesia, e273-e283. https://dx.doi.org/10.1016%2Fj.bja.2019.03.023
7. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators (2017). Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet, 1211–1259. https://doi.org/10.1016/S0140-6736(17)32154-2
8. Younger, J., McCue, R., & Mackey, S. (2009). Pain Outcomes: A Brief Review of Instruments and Techniques. Current Pain and Headache Reports, 39-43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2891384/
9. Asher, A. (2020). An Overview of Pain Management. Verywell Mind. https://www.verywellhealth.com/what-is-pain-management-296604
10. National Institute of Drug Abuse. (n.d). Opioids. National Institute of Drug Abuse. https://www.drugabuse.gov/drug-topics/opioids
11. Centers for Disease Control. (2021). Drug Overdose Deaths in the U.S. Top 100,000 Annually. Centers for Disease Control. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm
12. Drug Policy Alliance. (2020). Drug Overdose. Drug Policy Alliance. https://drugpolicy.org/issues/drug-overdose
13. Castellanos, J., Woolley, C., Bruno, K., Zeidan, F., Halberstadt, A., & Furnish, T. (2020). Chronic pain and psychedelics: a review and proposed mechanism of action
Highlighted Institutes
These are the institutes, from companies to universities, who are working on Pain.
Revixia Life Sciences
Revixia Life Sciences is a biotech company developing Salvinorin A (salvia) for substance use disorders (SUD), treatment-resistant depression (TRD), and pain.
Imperial College London
The Centre for Psychedelic Research studies the action (in the brain) and clinical use of psychedelics, with a focus on depression.
University of California San Diego
The Psychedelics and Health Research Initiative (PHRI) at UC San Diego conducts novel basic and clinical research on the use of psychedelics.
MindMed
MindMed is one of the largest companies in the psychedelics space and is developing various psychedelics for mental health disorders.
Bexson
Bexson Biomedical is developing an innovative preparation of ketamine to treat chronic and acute pain disorders.
Pharmather
Pharmather is a Canadian life sciences listed company that is developing psychedelics for brain and nervous system disorders.
Clusterbusters
Clusterbuster is a non-profit that supports research for better treatments and a cure while advocating to improve the lives of those struggling with cluster headaches.
Highlighted People
These are some of the best-known people, from researchers to entrepreneurs, working on Pain.
Peter Hendricks
Peter Hendricks is a Professor in the Department of Health Behaviour at the University of Alabama. Hendricks's area of expertise lies in substance abuse treatment and prevention.
Linked Research Papers & Trials
Pro & Business members will be able to see all linked papers and trials directly on this topic page.
This information is still available for you by selecting Pain on the Papers and Trials pages respectively.
See the information directly on this page with a paid membership.

