Effect Matrix of Psychedelics for PTSD
Key Insights about Psychedelics for PTSD
- PTSD generally occurs in people who have experienced or witnessed a traumatic event such as a serious accident, war/combat, or rape or who have been threatened with death or sexual violence. Four groups of symptoms exist: intrusive memories, avoidance, negative changes in thinking and mood, and changes in physical and emotional reaction.
- Thanks to the work of MAPS over the past 35 years, MDMA-assisted therapy for the treatment of PTSD is poised to be the first legally accessible Schedule I psychedelic-assisted therapy. It is estimated this could happen as early as late 2024.
What is PTSD?
Posttraumatic stress disorder (PTSD) is a psychiatric disorder that may occur in people who have experienced or witnessed a traumatic event such as a natural disaster, a severe accident, a terrorist act, war/combat, or rape or who have been threatened with death, sexual violence, or serious injury [1].
Although most people who experience traumatic events may temporarily struggle to adjust and cope, PTSD symptoms often last for months or years and interfere with day-to-day functioning.
PTSD symptoms are generally grouped into four types: intrusive memories, avoidance, negative changes in thinking and mood, and changes in physical and emotional reactions [2].
Symptoms in these four groups include recurrent, unwanted distressing memories of the traumatic event, avoiding thinking or talking about the traumatic event, negative thoughts about yourself or the world and being easily startled or frightened, respectively.
These symptoms vary from person to person and can vary in intensity over time. A person must experience symptoms for more than one month to be diagnosed with PTSD by a medical professional [1]. Furthermore, PTSD is generally grouped alongside anxiety disorders given the similar symptomology experienced.
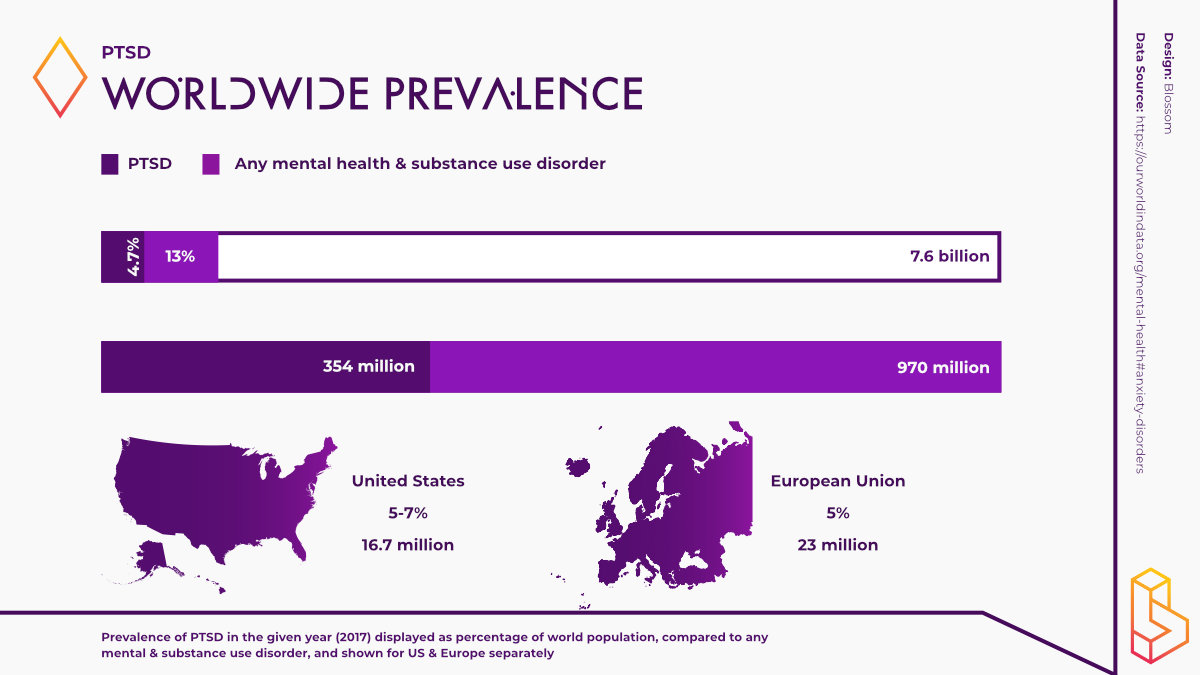
The global prevalence of anxiety disorders varies from 2.5 to 7% by country, making it one of the most prevalent mental health disorders [3].
It is estimated that there 354 million people suffering from PTSD globally [4]. This number is attributed to adult war survivors only. Thus, the global prevalence of PTSD is likely much higher.
Other mental disorders such as depression, anxiety and substance use disorder are often experienced comorbidly with PTSD, making it a disorder that can be difficult to treat [2].
Conventional PTSD Treatment
PTSD is often a chronic condition despite the availability of various evidence-based treatment options [5]. Conventional treatments for PTSD vary from person to person.
The main treatments for people with PTSD are medications, psychotherapy, or both. Different forms of therapy exist but they share the same goals such as teaching a person about trauma and its effects, using relaxation and anger-control skills, and changing how people react to their PTSD symptoms [6].
For example, cognitive processing therapy (CPT) is one form of psychotherapy used to treat PTSD. CPT is usually delivered over 12 sessions and helps patients learn how to challenge and modify unhelpful beliefs associated with the trauma.
In prolonged exposure therapy (PET), after initial assessment by a medical professional, patients are exposed to anxiety-provoking thoughts and images which the therapist helps them to process in a safe environment.
Several types of medications exist to help improve symptoms of PTSD, with antidepressants (SSRIs) being the most studied. The SSRIs paroxetine and sertraline are FDA approved for PTSD treatment [2]. Moreover, anxiolytics may be used to relieve severe anxiety however, they are generally used for a short period given their abuse potential.
Psychedelics and PTSD
MDMA and PTSD
Rick Doblin, the founder of MAPS and one of the most well-known names in the world of psychedelics, and the team at MAPS carried out the first double-blind, placebo-controlled trial of MDMA-assisted psychotherapy for PTSD in 1994.
Since then, MAPS have continued to explore this avenue and a plethora of trials have taken place and are continuing to emerge across the globe investigating the potential of psychedelics, particularly MDMA, to treat PTSD.
Largely based on roughly 30 years of work by MAPS, the preliminary evidence demonstrating the ability of MDMA to help those with PTSD led to MDMA being awarded breakthrough therapy status by the Food and Drug Administration (FDA) for the treatment of this disorder.
Another factor leading to this designation is the demographic of participants in these clinical trials: the majority being veterans of war. According to a 2017 study, PTSD is nearly twice as prevalent in veterans when compared to the general population in the US [7].
Since its breakthrough designation, MAPS have continued to work relentlessly toward getting MDMA approved by the FDA. Their work is now starting to bear fruit as the therapeutic potential that MDMA is demonstrating combined with the high prevalence of PTSD, particularly in veterans, means that MDMA may become the first Schedule I psychedelic to be granted FDA approval. This could happen, if all stars align, as soon as 2023.
Researchers at MAPS conducted six Phase II trials using MDMA-assisted therapy to treat PTSD. Across the studies, researchers observed significant and sustained decreases in PTSD, measured using the most widely used PTSD scale, CAPS-5.
A pooled analysis of the results of these six trials showed MDMA-assisted therapy had a very large effect, with 56% of participants no longer meeting the criteria for PTSD. Moreover, improvements in symptoms were sustained 1 to 3.8 years post-treatment.
Following the success of the Phase II Trials, MAPS recently carried out the world’s first Phase III clinical trial into MDMA-assisted therapy for PTSD. Led by Jennifer Mitchell, the trial consisted of 90 participants and took place across 15 studies in the US, Canada, and Israel. Participants underwent three preparatory therapy sessions and nine integrative therapy sessions following three experimental sessions with MDMA.
MDMA (8-120mg) was found to induce a significant and robust reduction in CAPS-5 scores compared with placebo. 67% of participants in the MDMA group no longer qualified for PTSD while this figure was 32% in the therapy-only group. Adverse events in the MDMA group were typically transient and mild to moderate in severity.
MAPS is continuing to sponsor a range of trials in the US and Europe exploring the potential of MDMA to treat PTSD.
As of January 2022, MAPS has been granted an Innovation Passport in the U.K for MDMA as an adjunct to therapy for PTSD. While this designation does not reduce the need for MDMA to demonstrate both safety and efficacy, it aims to accelerate the drug development process by providing researchers with expert advice, patient input and collaboration throughout the clinical trial design and development process.
Ketamine and PTSD
Ketamine is another psychedelic that is being trialled in the treatment of PTSD.
Adriana Feder and colleagues (2014) compared the efficacy of ketamine (35mg/70kg) to midazolam (3.15mg/70kg) for treating PTSD and the depressive symptoms associated with the disorder. Ketamine was associated with a significant reduction in PTSD symptom severity compared to midazolam, assessed 24 hours after infusion. A reduction in depressive symptoms was also observed.
Adrian Feder and colleagues have continued to explore this potential use of ketamine. In a 2021 study, the researchers assessed the effectiveness of repeated ketamine infusions (6x, 35mg/70kg) compared to midazolam for PTSD. 67% of participants in the ketamine group were treatment responders, compared to 20% in the midazolam group. The positive effects of ketamine faded, on average, within a month.
While the results of these trials are positive, the findings of the largest study to date exploring the effectiveness of ketamine to ameliorate symptoms of PTSD tell a somewhat different story.
In this study, 158 veterans and active service members were randomised to three groups: standard ketamine dose (n=51, 35mg/70kg), low ketamine dose (n=53, 14mg/70kg) and placebo (n=54, saline). Participants received ketamine or placebo twice per week for four weeks yielding a total of eight dosing sessions.
The trial failed to find a significant dose-related effect of ketamine on symptoms of PTSD over the 4-week study duration. Thus, these findings do not support the use of PTSD in veterans and active service members. However, a significant reduction in depressive symptoms was observed in this group.
While the demographics of the study populations in these trials may help to explain the difference in findings, it is too early to tell if ketamine is an effective (and durable) treatment for PTSD.
Mescaline and PTSD
Mescaline remains relatively understudied in the world of psychedelic medicine. While it has been used for religious purposes by Indigenous communities in the Americas for centuries, clinical trials with mescaline are yet to take place. The limited data on this substance tends to come in the form of survey studies and anecdotal reports.
In terms of mescaline being used to treat PTSD, a survey study found that it improved symptoms of the disorder. The anonymous online survey of 452 adults who reported mescaline use in naturalistic settings found that 76 per cent of people who reported experiencing PTSD symptoms (n=55), accredited the use of mescaline with improvements in their symptoms.
Other psychedelics
Another survey study (n=51) assessed the effects of ibogaine and 5-MeO-DMT treatment in U.S Special Operations Forces Veterans who had sought treatment with these substances in Mexico. The results indicated significant and large reductions in symptoms of PTSD as well as suicidal ideation, depression and anxiety. Nonetheless, controlled studies will be needed before any definitive conclusions can be drawn.
How might psychedelics treat PTSD?
For most psychedelics, their exact mechanisms of action remain speculative. Some believe that psychedelics like MDMA “reopen” critical periods, which are certain time windows of optimal learning as animals and humans grow from infancy to adulthood.
By reopening these critical periods, psychedelics could prime the brain to reorganize and adjust the meaning of a traumatic memory or unhealthy thought pattern [8].
MDMA differs from classic psychedelics like psilocybin and DMT, causing it to be classified as an entactogen. Entactogens are psychoactive substances that produce experiences of emotional communion, oneness, relatedness, and emotional openness.
MDMA acts on the brain by stimulating the release and blocking the reuptake of mainly the neurotransmitter serotonin – making it more ‘available’ in the brain. It does this also for dopamine and norepinephrine to a lesser degree [9].
By elevating these levels of neurotransmitters in the brain people feel more open, have a greater sense of empathy, sensory pleasure, and less anxiety [10].
In this state of openness, experts have found that people with PTSD can work through traumatic events more effectively with their therapist.
In the MAPS studies with MDMA for PTSD, the importance of the therapeutic component of therapy is emphasized. Integration sessions are needed with a therapist following the psychedelic experience in order to gain the full therapeutic benefit from MDMA.
Ketamine, on the other hand, is an NMDA receptor agonist. By binding to these receptors, ketamine stimulates the release and inhibits the reuptake of the neurotransmitter glutamate. This causes synapses to form and fire and strengthens neuronal activity, which may account for, in part, ketamine’s therapeutic effects.
Interestingly, in the trials using ketamine to treat PTSD, no therapy is given. Thus, it could be worth exploring the effects ketamine has on symptoms of PTSD when therapy is also given.
Psychedelic Companies and PTSD
Numinus Wellness is a Vancouver-based company focusing on using MDMA-assisted therapy to treat PTSD. In partnership with MAPS, Numinus was recently granted approval by Health Canada for an open-label study for MDMA-assisted therapy for PTSD. This study aims to assess the safety and feasibility of using MDMA to treat PTSD.
Led by Dr. Devon Christie, Medical and Therapeutic Services Director at Numinus, the study has been granted ethics approval and is preparing to enrol participants as of January 2022.
New York-based company Seelos Therapeutics is currently developing an intranasal spray for administering ketamine, known as SLS-002. Seelos hopes that the following approval, SLS-002 will be available to patients with PTSD, major depressive disorder, or both.
Given the immense amount of time and effort MAPS have invested in making MDMA a viable treatment option for those with PTSD, it is likely that they will continue to be the most important company in this area of psychedelic medicine.
While they have launched MAPS PBC, their for-profit subsidiary, it is worth noting that MAPS have been able to get this far operating as a non-profit that largely relies on donations, particularly in light of the ongoing profitability/patent debates dominating the psychedelic discourse.
MAPS have recently partnered with Vine Ventures to pioneer a social impact Special Purpose Vehicle, called Regenerative Financing Vine (RFV) that will see $70 million incorporated into patient access infrastructure and research for MDMA-assisted therapy for PTSD. The RFV ensures that revenue generated from MDMA-assisted therapy remains available to fund MAPS’ non-profit mission and MAPS PBC’s public benefit drug development activities.
As research in this area of psychedelic science progresses, it is likely more companies will enter this space with novel formulations of various psychedelics in the hope that they can be used to successfully treat PTSD. Overall, the future looks very promising for people with PTSD in need of novel and effective treatments.
External references for PTSD and Psychedelics
All resources available on Blossom are directly linked on this topic page. Find even more background about this topic with these external references.
1. American Psychiatric Association. (2020). What Is Posttraumatic Stress Disorder? Washington DC: American Psychiatric Association. https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd
2. Mayo Clinic. (2018). Post-traumatic stress disorder (PTSD). Rochester: Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/post-traumatic-stress-disorder/symptoms-causes/syc-20355967
3. Dattani, S., Ritchie, H., & Roser, M. (2021). Anxiety Disorders. Our World in Data. https://ourworldindata.org/mental-health
4. Hoppen, T., & Morina, N. (2019). The prevalence of PTSD and major depression in the global population of adult war survivors: a meta-analytically informed estimate in absolute numbers. European Journal of Psychotrumatology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6394282/
5. Vermetten, E., Krediet, E., Bostoen, T., Breeksema, J., Schoevers, R., & van den Brink, W. (2020). Psychedelics in the treatment of PTSD. Tijdschrift Voor Psychiatrie, 640-649. http://www.tijdschriftvoorpsychiatrie.nl/en/issues/555/articles/12296
6. National Institute of Mental Health. (2019). Post-Traumatic Stress Disorder. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd
7. Muller, J., Ganeshamoorthy, S., & Myers, J. (2017). Risk factors associated with posttraumatic stress disorder in US veterans: A cohort study. Plos One, e0181647. https://dx.doi.org/10.1371%2Fjournal.pone.0181647
8. Frysh, P. (2022). How Do Psychedelic Treatments Work? WebMD. https://www.webmd.com/mental-health/story/how-do-psychedelic-treatments-work
9. National Institue on Drug Abuse. (2017). What are MDMA’s effects on the brain? National Institue on Drug Abuse. https://www.drugabuse.gov/publications/research-reports/mdma-ecstasy-abuse/what-are-mdmas-effects-on-brain
10. WebMD. (2021). MDMA-Assisted Therapy for PTSD: What to Know. WebMD. https://www.webmd.com/mental-health/what-is-mdma-assisted-therapy-ptsd
Highlighted Institutes
These are the institutes, from companies to universities, who are working on PTSD.
Healing Breakthrough
Healing Breakthrough is a non-profit organization dedicated to addressing the urgent need for improved treatment options for veterans suffering from post-traumatic stress disorder (PTSD).
Remedy
Remedy is a psychotherapy clinic and research group helping people living with a range of mental health disorders.
MAPS
MAPS stands for Multidisciplinary Association for Psychedelic Studies, it's the front runner in making psychedelics a legal way to use (and improve) in therapy.
MAPS PBC
MAPS Public Benefit Corporation (MAPS PBC) is the 'benefit above profit' corporation that is fully owned by MAPS.
Numinus
Numinus is a Canadian company trying to create a platform for the therapeutic use of psychedelics. Working together with researchers, yet also wanting to see how to make it commercially viable. The two founders both came here from personal experiences.
Highlighted People
These are some of the best-known people, from researchers to entrepreneurs, working on PTSD.
Marc Capobianco
Marc is a psychiatrist specializing in post-traumatic stress disorder, depression, obsessive-compulsive disorder, schizophrenia, and mood disorders.
Cristina Albott
Cristina Albott is a psychiatrist who treats patients in need of mental health care. She is currently leading a trial investigating the effectiveness of repeated ketamine infusions in veterans with PTSD and comorbid depression.
Anne Wagner
Anne Wagner is the Founder of Remedy, a clinical psychologist and treatment development researcher based in Toronto.
Rick Doblin
Rick Doblin Ph.D. is the founder of MAPS. His persistent work since 1986 has been one of the main drivers behind why psychedelics (including MDMA) are now coming back to therapy.
Linked Research Papers & Trials
Pro & Business members will be able to see all linked papers and trials directly on this topic page.
This information is still available for you by selecting PTSD on the Papers and Trials pages respectively.
See the information directly on this page with a paid membership.