This post synthesises my (Floris Wolswijk) LinkedIn posts on psychedelics through the Effective Altruism lens; follow along for more.
Are psychedelics effective interventions for mental health?
Many would say yes, but does it hold through the Effective Altruism lens?
First, what is effective altruism (EA)? It is a movement that tries to do as much good as possible. How? Through using evidence and reason.
For example, it compares global health charities and looks at where donations will go the furthest.
Those who engage with EA call themselves effective altruists. I count myself as one of them. Specifically, I donate 10% of my income and have organised a local EA group for six years.
So, where do psychedelics fit within this picture? Can psychedelics as medicines be an effective intervention for mental health? Do we have evidence for this?
In this essay, I will try and answer this through the four pillars of an EA framework:
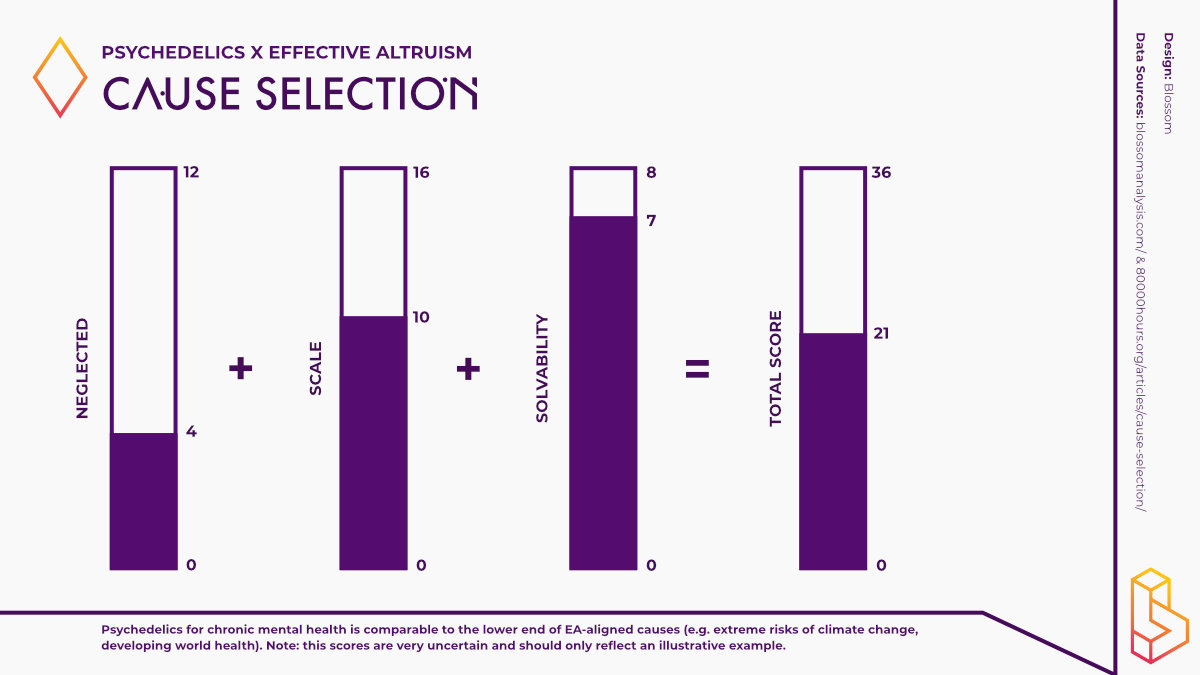
- Neglected – How many resources are already going towards solving this problem?
- Importance (scale) – How good would it be if we solved this problem?
- Tractability (solvability) – How much better would things get if we throw more resources at the problem?
- Personal fit – Given your skills, resources, etc. – How likely are you to excel in this area?
Though far from an exact science, the answers to the first three questions will make the area of ‘psychedelics as medicines’ comparable to other fields. The final question helps indicate if you should work directly in the domain.
Is psychedelic science neglected?
A billion dollars* later, can we still answer yes?
Neglectedness, from an EA perspective, stands for the relative lack of resources already going toward solving a problem. If many resources are going towards a problem, the low-hanging fruits are more likely to be picked.
For example, billions flow towards solving cancer in kids (a great cause) but much less towards preventing malaria (a neglected cause).
Researchers investigate psychedelics for various topics, ranging from psychedelic-assisted therapy for treatment-resistant mental health issues to non-hallucinogenic interventions for chronic pain. To say something useful about neglectedness, I must specify further. For the sake of this series, this is the question: How many people, or dollars, do we currently dedicate to solving ‘treatment-resistant’ (chronic) mental health disorders?
As a percentage of total health spending, governments spend between 0% and 12% on mental health. The US spends about 5% ($225 billion) of the health budget on mental health. A quarter of countries spend less than 1% of health money on mental health. The lack of spending on mental health, which is more prevalent in low- and middle-income countries, is referred to as the ‘treatment gap’.
The number of people working on mental health varies from <1 to ~100 per 100.000 inhabitants. Of these, nurses make up the bulk and psychiatrists the smallest number.
The two previous paragraphs help paint a picture of total investment in mental health but don’t specify how much we spent on treatment-resistant disorders. To be frank, it’s challenging to disentangle the numbers. From a scale perspective (covered below), the healthcare costs of someone with treatment-resistant depression are twice that of depression and quadruple that of someone without a diagnosis.
Through the lens of neglectedness, I can argue that of the healthcare budget, much of what we spend on research is not directly helping those affected by mental health disorders. But how much is spent directly on trying to solve treatment-resistant mental health disorders? I can’t say yet.
Going back to the EA framework, I estimate that we spend at least $1 billion annually on solving chronic mental health issues. Similarly, at least 10.000 people are working on this. This data gives us a neglectedness score of 4 (0 = neglected, 12 = crowded). You can convince me that the actual score is lower (a 2 or 3) if there is more reliable data on these numbers.
The neglectedness score is thus not very high compared to other cause areas. For instance, factory farming scored a 6 (investments of $100 million), and investments in risks of AI scored an 8 ($50 million, 300 people working directly in the area).
Are psychedelics as medicines solving something important?
10% of the world battling mental health problems wholeheartedly say YES.
If we (partially) solved ‘treatment-resistant’ (chronic) mental health disorders, by how much would the world become a better place?
To know how much improvement there theoretically can be, we first have to know the current negative impact of mental health disorders.
Worldwide, 10% of the population (18% in the US) is battling mental health issues. That is 800 million people, rising to 1 billion if we include substance use disorders.
Put into dollars, the US spends $280 billion on treatments. The loss to the global economy (by people not working due to mental illness) is $2-5 trillion. Put more bluntly, this is a big fucking deal, and we’re not spending enough on solving it.
The economic costs of someone battling chronic depression are four times that of the average person ($20k vs $5) or double that of someone with an episode of depression ($10k). The numbers include direct (healthcare) and indirect (productivity lost) costs but gloss over mental health issues’ vast impact on friends and family.
An estimated third of the economic loss from mental health comes from chronic illness, putting the potential savings at $700 to $ 1.700 billion.
Another perspective on importance measures the years of good life lost (DALY, disability-adjusted life years, QALY is the inverse – years of good life gained). Each year, mental health disorders lead to 125 million DALYs. If we again take a third of these to be attributed to chronic conditions (which I think is conservative), we get 40 million DALYs.
Plugging this into the EA framework, we get a scale of 10 (out of 16). Solving chronic mental health disorders for which we don’t currently have suitable treatments is paramount.
This score could be even higher if we consider the positive spillover effects. We have neatly divided mental health into boxes, but anyone with some life experience knows this isn’t how the world works. A person might also stop smoking, fighting, or start the next Google when their mental state improves.
So far, I’ve discussed the neglectedness and scale of chronic mental health disorders. Now it’s time to bring in psychedelic treatments themselves. Do they have a shot at solving this?
Are psychedelics as medicines a solution for chronic mental health?
Studies point towards yes, but what about our certainty if we scale up?
If we doubled direct effort on ‘treatment-resistant’ (chronic) mental health disorders, what fraction of the remaining problem would we expect to solve?
Here is where the rubber meets the road. Can the investment in psychedelics as medicines have a sizeable impact on solving chronic mental health disorders?
Putting this into the EA framework, I would give it a solvability score of 7 out of 8 (between 10-100% chance of solving/successfully treating chronic mental health disorders).
If we look at investments in mental health, two patterns emerge:
- Spending more money (doubling of mental health budget over ten years) hasn’t had any impact (things have gotten worse)
- (Some/Individual) Mental health interventions have an incredible ROI, and we’re underinvesting in them
Studies with psychedelics show effectiveness for treating chronic mental health disorders from 20% (Compass, Phase IIb) to 67% (MAPS, Phase IIIa). Psychedelic-assisted therapies present a novel framework for tackling the most difficult-to-treat populations. We, who are invested in the field, see an island of hope in these treatments.
But, the studies are still tiny, with the Compass study being the largest to date (n=209 completion, a third in the active treatment arm). The much debated ‘hope and hype’ might be responsible for much of the effects seen in clinical trials.
Founders Pledge (an EA-aligned organisation) used Bayesian analysis to correct for the hype seen in early trials. Without going into the details, their estimate of a reduction in depression scores (HAM-D) is 2.19 points (>23 points is severely depressed), so a relatively minor reduction.
The real-world effectiveness of psychedelic-assisted therapies is thus still an open question. Only after next year (MAPS‘ Phase IIIb) and in 2026 (Compass’ Phase III) can we know with more certainty.
But other hurdles await us. Legislation (remember, we are talking about Schedule I drugs) and costs (reimbursement) are two topics I’ll cover on another date. What I can say now is that a significant uphill battle awaits.
Still, assuming these two (of many) problems are solved, I think it’s not unreasonable to presuppose more than 10% of those treated with psychedelic-assisted therapies will find long-term relief from them.
Before I cover personal fit, let’s add up the (very uncertain) scores that we’ve gotten: 4 (neglected) + 10 (scale) + 7 (solvability) = 21. Psychedelics for chronic mental health is comparable to the lower end of EA-aligned causes (e.g. extreme risks of climate change, developing world health).
Should you be working on psychedelics as medicines?
In the previous sections, I assessed if psychedelics as medicine (focusing on chronic mental health conditions) is the place on which to work.
Here I’ll answer: given your skills, resources, knowledge, connections and passions, how likely are you to excel in this area?
This section is more personal. I hope my example will inspire you to answer the same (sub) questions.
When I came into the field of psychedelics as medicine, I brought with me three sets of skills.
- Master’s (MSc) in psychology (I could grasp the background knowledge implied in research articles)
- A big bag of general entrepreneurial skills from running a company for five years (self-starter, curious, and comfortable with uncertainty
- Know how to build a website (more specific skills for what I did with Blossom)
- Bonus: ~100 experiences with psychedelics
A good friend of mine is a psychedelic researcher, but besides him, I knew no other person working on this directly (in other words, a connection, but I firmly believe you can make these whilst exploring).
Next to this, I have an intense curiosity (passion) for psychedelics. I see in psychedelics a way to have a massive impact on the world whilst also applying and developing my skills. In other words, my motivation is high (pun intended).
With my entrepreneurial background, I see an opportunity to fill an informational gap (making research accessible & applicable), and my specific role could be to fill that gap (and excel at doing that).
I believe I can have an outsized impact (have an influential role) by providing what I do at Blossom. And that over the past three years, continuing onward, I can keep building my career capital to execute this vision.
If you’re likely to excel with your background, I can’t answer for you. What I can motivate you to do is to explore (this field or another) and answer these questions for yourself.
One tip I want to give you right now is to speak to people doing the job you want. I’ve talked to tens of people who are interested in the field and have felt inspired after each conversation. Similarly, I’ve reached out to people and always enjoyed learning from them.
If there is anything to take away from this essay: reach out to someone doing the thing you want to do.
If you want to hear me speak about this (digitally), visit EAGxRotterdam on 4-6 November 2022.
*Over a billion has been invested in psychedelic startups. Not all of that money – or not even half of it – has gone directly to supporting research. For more, see Psychedelic Alpha.
Become a psychedelic insider
Get a Pro Membership to enjoy these benefits & support Blossom📈 full reports on Topics & Compounds
🧵 full summary reviews of research papers
🚀 full access to new articles
See Memberships