Key Insights
- Cultural Context Matters: Psychedelic use in religious and cultural contexts, such as among Amazonian indigenous groups in Brazil, is accepted and considered beneficial for intellectual and spiritual enlightenment. This contrasts Western perspectives, which often stigmatize psychedelic use, especially among adolescents, as dangerous or indicative of substance abuse.
- Scientific Research Challenges Stigmas: Ritualistic use of psychedelics like ayahuasca or psilocybin may positively affect mental health. For example, adolescents who were regular ayahuasca consumers within their religious communities showed a lower risk for psychiatric symptoms than controls. This challenges the prevailing Western notion that psychedelic use is inherently harmful, especially for young people.
- Therapeutic Potential is Underexplored but Promising: Psychedelics are increasingly being considered for their therapeutic benefits in treating mental illnesses like PTSD and depression, even among adolescents. While the research is still in its infancy, early findings are optimistic, suggesting that psychedelics could be a valuable tool in psychotherapy and mental health treatment, contradicting their demonized reputation in some Western societies.
Author: Natasha Ng. Natasha is a psychology student from Macquarie University studying Cognitive Neuroscience. She’s worked with Blossom to compile the information on psychedelics and adolescents on this topic page.
Novel Explorations of Psychedelic Use in Adolescents
It may be unsettling to Western societies that children and adolescents use psychedelics. The problematic outcomes of such an activity have long been associated with the development of psychological disorders or a substance abuse habit. However, contemporary psychedelic science may very well challenge these presumptions through the exploration of intercultural practices. Such practices endorse psychedelic use as a normality for young people to consume.
This topic page explores the studies reporting on psychedelic use in a religious context related to the health and well-being of children and adolescents (aged 10-19). Such findings will be analysed against the emerging research of psychedelic use by young people – in both recreational and Western medicinal contexts – to enliven a discussion about the perspectives relating to psychedelic use in young people.
Psychedelics, Anthropology, & Religion
Psychedelic consumption occurs in cultural contexts throughout the world. Religious perspectives explain why believers, who may sometimes be adolescents or children, can consume these substances. In the context of Amazonian indigenous groups in Brazil, a psychoactive mix of Banisteriopsis caapi and Psychotria viridis is used in shamanic rituals. Otherwise referred to as ayahuasca, daime, hoasca, or vegetal; these Amazonian plants of interest often contain dimethyltryptamine (‘DMT’), which induces a powerful psychoactive experience.
To understand the religious reasons for the use of ayahuasca, a series aired by National Geographic called Taboo reported on the practices of the Santo Daime community of Centro Eclético da Flor de Lótus Iluminado who reside in the Brazilian state of Acre. Controversially, the segment recorded infants and children consuming ayahuasca, as well as pregnant women. Accordingly, these religions afford legal recognition to ayahuasca consumption and endorse its social legitimacy because it is believed that the psychedelic can offer intellectual enlightenment from physical or mental suffering [1]. Motivations to consume ayahuasca include the possibility of accessing greater knowledge, an enhanced state of consciousness and healing capabilities of the self and others [2]. In addition to other various lifestyle habits, shamanism inspires religious communities to consume ayahuasca in the hope of attaining self-healing and divination.
Psychedelic consumption in remote indigenous communities remains a limited area of research for anthropologists and scientists. Xavier Da Silvera and colleagues explored a preliminary psychiatric assessment of the health of adolescents who had been regular ayahuasca consumers within their religious communities. Forty participants were from a Brazilian religious group, and 40 controls were matched by age, gender and educational background. The study explored if adolescent ayahuasca users were more likely to report psychiatric disorders such as depression, anxiety, alcohol consumption or body dysmorphia. Standardised reporting instruments such as the Self Report Questionnaire to assess overall psychic condition, the Center for Epidemiological Studies Depression Scale, the Beck Anxiety Inventory, the Drug Use Screening Inventory, and the Body Shape Questionnaire were used. The results noted a lower risk for participants who were regular ayahuasca users to display psychiatric symptoms. Therefore, these users may be considered ‘healthier’ compared to controls, which could be surprising to some considering the looming stigma surrounding psychedelic use.
Further, Doering-Silveira and colleagues focused on ayahuasca consumption in adolescents who had been using the substance in a ritualistic context at least twice a month in the 24 months preceding the study. Forty-one of these participants were evaluated against 43 non-users. However, in this instance, both groups were part of the same community and subject to the same environmental influences. The aim was to determine whether one group had a higher risk of drug misuse. Regarding misuse, the study’s findings favoured ayahuasca consumers, observing that they were considered more confident, persistent, and reflective. However, a caveat to these findings is that controlled studies on the mental and psychiatric standing of religious and ceremonial hallucinogen consumers is scarce. Therefore, it is worth noting that low frequencies of psychiatric symptoms in adolescents could be influenced by other religious affiliations or influences that have not yet been accounted for in scientific explorations. External influences such as a strong sense of belonging to a structured religious community or a rigid belief system may act as a protective mechanism for substance use disorders or other psychiatric illnesses.
Psychedelic Use by Adolescents in Western Societies
From an alternative perspective, psychedelic use by adolescents in the Western world has attracted attention from researchers. This interest is twofold, one exploring the use of psychedelics by adolescents for recreational purposes and the other exploring their use for medical purposes.
Recreational use of psychedelics in a Western context
Adolescents who use psychedelics within a recreational context have been reported lightly in the existing literature. Often, the media and internet materials can use science to demonise the effect of drugs on the neurological health of vulnerable people, particularly adolescents. For example, Singer and colleagues conducted a study on the psychosocial profiles of adolescents using MDMA, noting the frequent reason for use occurs in a ‘party/club’ environment [3]. It was hypothesised that MDMA users would be subject to ‘negative consequences’ as opposed to non-MDMA users. The consequences observed for MDMA users included an increased risk of drug abuse and use of other drugs, as well as impairments to social and familial relationships. The quantitative data collected from user reports also showed a higher rate of functional problems in daily life in tasks such as academic performance. The relevance of functional problems that affected MDMA users contradicts the view advocated for by Koesters and colleagues, who present MDMA as a benign drug promoting emotional warmth, empathy and healing from psychiatric disorders [4]. Users also self-reported more experiences of childhood trauma and elevated levels of depression. Despite these outcomes, this study is limited by the participants’ demographic (i.e. Western adolescents of the same age who were in the same life stage and were already frequent users of other drugs affecting personality). Accordingly, the correlational findings must not be confused with determining causation.
To consider whether recreational use of psychedelics by adolescents is detrimental to the development of neurocognitive functions, a 2004 study by Jacobsen and colleagues tested for evidence of cognitive deficits and alterations to brain functioning in adolescent MDMA users [5]. The study utilised fMRI and statistical analysis to neuroimage six participants who were frequent users of MDMA against six controls who were non-users. The method for testing the effects on cognitive load was explored through a series of selected and divided attention tasks, which call on the brain’s capacity to increase its activation of the left hippocampus. Notably, MDMA users exhibited reaction times that were significantly prolonged and lacked the subsequent activation of the left hippocampus. This study was correlational, so it may be possible that other factors affecting the condition of the users’ brains could have caused neurotoxicity. Therefore, larger studies are required to substantiate the findings and confirm whether the adolescent brain is significantly affected by MDMA use.
Adolescents may frequently consume MDMA, dissociatives and classic psychedelics. Bates and Trujillo explain that adolescence promotes an increased chance for individuals to engage in risk-taking behaviours [6]. These behaviours can involve impulsive decision-making caused by a degree of curiosity. In the 1960s and 70s – when ketamine and PCP were used for medical procedures – their popularity as recreational drugs also emerged. These atypical psychedelics cause consumers to experience a euphoric rush with other sensory distortions and feelings of numbness. The popularity of dissociatives among young people increased in the 2000s, particularly in the context of raves or dance clubs. Looking at the statistics that have emerged, the lifetime use of PCP in 2015 was 2.4% (approximately 6.3 million people in the US), where the average age of introduction to this drug was 15.3 years. For ketamine, adolescents were generally introduced to it at subanesthetic doses at around the age of 19.6 years. The context in which these dissociatives have been reported to be commonly consumed, the general environment, and ‘pleasurable’ episodes that adolescents have reported have often been correlated with addictive behaviour and long-term use [7].
Medical use of psychedelics in a Western context
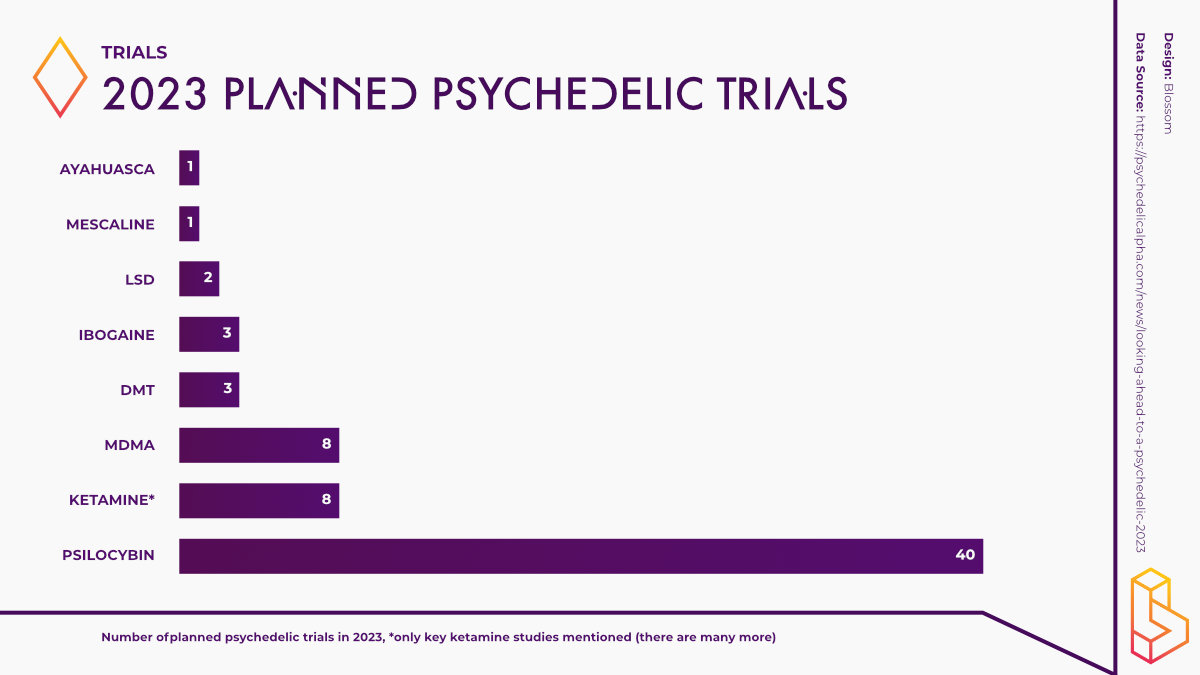
Alternatively, psychedelic use has been extensively reported in medicine. This area of research is relatively novel and emerging. Psychedelics have offered promising results for treating multiple mental illnesses, with psilocybin being the most commonly explored substance in 2023 (see graph). In this context, MDMA has been proposed as a tool in psychotherapy that may assist in treating adolescents suffering from post-traumatic stress disorder (PTSD). Van Vugt and colleagues collated the perspectives of adolescents, parents and clinicians about the potential for clinical application of MDMA-assisted psychotherapy (MDMA-AT).
To date, however, no trials have been conducted with MDMA-AT for PTSD in adolescents, but nonetheless, the perspectives offered by participants are interesting. Results included initial apprehensive and unfavourable perspectives of MDMA use to treat PTSD in adolescents, except for those who were themselves adolescents and had conducted their own research prior. However, once an explanation of the drug’s prospects was explained, all (19) but one of the participants changed their minds and supported the idea. Rick Doblin, the founder of MAPS (Multidisciplinary Association for Psychedelic Studies), has consistently advocated for the therapeutic use of psychedelics and their potential rehabilitative benefits. As we progress towards a more pragmatic future, the use of MDMA to treat anxiety and other stress disorders allows for the previously demonised account of recreational drugs to be re-evaluated. As we have seen, once informed, parents, clinicians and adolescents can agree with this proposition.
In discussion with one of the authors, Josjan Zijlmans noted that initial perceptions by people often tend to embody a “simplistic view” that “drugs are bad”. However, their views can be “fairly flexible with proper information”. This is because often, there may be a lack of knowledge about how substances that are used recreationally can have a purpose in a medical context. When asked about the influence of a ‘party drug pandemic’ on this view, Zijlmans replied that it might not be as influential as initially thought. For example, he noted that in the Netherlands, “drug use is fairly stable”, a topic that is less taboo and afforded more media attention for its clinical prospects. The role of researchers in the media was also discussed. Zijlmans proposed that researchers should share more of their work with the media and be active in public debates concerning their area of expertise. Recently, in his hometown of Rotterdam, there has been an ad campaign against drug use, which Zijlmans notes may be “ineffective or even counterproductive”. The usefulness of this input brings another perspective to the debate that helps to balance competing perspectives.
Psilocybin is a substance that has been researched for its medicinal properties in various contexts. Bogadi and Kaštelan reported on one participant who was at a psychiatric clinic to treat social anxiety and poor school performance [8]. This individual was 16 years old and administered 2 grams of psilocybe mushrooms thrice during an 18-month course. Remarkably, the patient reported a rapid change in symptoms after taking psilocybin. This included being motivated to accept feelings of pleasure and avoid discomfort.
The therapeutic effects of psilocybin have also been explored by Shah and colleagues, who recorded 172,745 adolescents’ experiences with the psychedelic [9]. The aim was to observe any trends experienced by young drug users. Of the sample population, 170,276 had never used psilocybin in their lifetime, whilst 2469 had. Of those who had experienced the substance, they were, on average, 17 years old and of non-Hispanic white backgrounds. The findings demonstrated that 31% of the users had lifetime major depressive episodes as opposed to 16% of the non-users. Whilst there may have been significant associations between psilocybin use and major depressive episodes among adolescents, the limitations of this study (i.e. the selective category of participants with little to no diversity in life experiences) warrant the need for caution to be taken when considering the findings.
Interestingly, a study by Jones and colleagues published findings the opposite [10]. In this context, MDMA, alongside other classic psychedelics such as psilocybin, were investigated from a sample of 262,617 survey participants. The study accounted for demographic factors and variables expanding beyond just sex and age also to include income, race, and education. Qualitative findings concerning adolescent suicidal thoughts and behaviours (STBs) were gathered. The results differed according to the type of psychedelic consumed. In relation to lifetime use of psilocybin, participants reported significantly lower odds of STBs. This finding reported a similar outcome to Jones and Nock, who found that lifetime psilocybin consumption is associated with reduced odds of past psychological distress occurring in the previous month or suicidal thinking within the previous year. However, despite the findings of these papers, such studies can’t be used to establish a causal relationship between psychedelic use and STB in adolescents. Instead, these studies offer important insights into the progression of psychedelic research and the potential for future cross-sectional, longitudinal and clinical investigations.
Among the most commonly studied substances is ketamine. Ketamine has been shown to have antidepressant effects on adults, but this is less widely explored in the case of young people and children. The potential clinical applications of ketamine to treat paediatric depression were studied by Meshkat and colleagues. This review focused on 46 participants (mean age of 16 years old) who were administered either 35mg/70kg or 140-490mg/70kg of intravenous ketamine. Notably, ketamine was significantly correlated with reduced depressive symptoms, without any severe consequences. However, the limitations in the sample size and the exploration of one method of administration (i.e. intravenous) results in a need for larger samples and different administration modalities to support such findings.
In cases of treatment-resistant depression (TRD), the proposed clinical application of ketamine was explored by Cullen and colleagues. In a sample of 13 participants, the efficiency and tolerability of ketamine in adolescents with TRD showed that only at higher doses could dissociative and hemodynamic symptoms diffuse and predict a treatment-like response. Ongoing neurodevelopment and the potential for neuroplasticity in adolescents and children make the clinical application of ketamine to treat depression in this category promising.
Are Psychedelics Bad for Adolescents?
This topic page has collated only parts of the plethora of research available in this area more broadly, focusing on children and adolescent participants. Considering the differences between Western and traditional cultural perspectives towards psychedelics, it can be challenging to determine where its therapeutic potential lies in modern science.
It has been explored that religious views embedded in an interconnectedness with spirituality, culture and tradition offer insight into the potential for psychedelics to enhance ritual experiences and a state of consciousness capable of healing oneself. Western societies have reflected such possibilities in results that reflect better states of psychiatric health or reduced possibilities of psychiatric ill-health.
However, when assessing the views of some Western societies, many offer a demonised record of psychedelic experiences. There is an unwillingness for these substances’ therapeutic and clinical use to prevail against their commonly perceived recreational ‘misuse’.
Nonetheless, it can be argued that the trials conducted so far are promising. Although they possess limitations and need further substantiation, their potential as a tool in psychotherapy and self-development is grounded, optimistic and currently undervalued.
External references for Adolescents and Psychedelics
All resources available on Blossom are directly linked on this topic page. Find even more background about this topic with these external references.
1. Walubita, T. (2020, February 21). Cultural Context and the Beneficial Applications of Ayahuasca. Lake Forest College. https://www.lakeforest.edu/news/cultural-context-and-the-beneficial-applications-of-ayahuasca
2. Fotiou, E., & Gearin, A. K. (2019). Purging and the body in the therapeutic use of ayahuasca. Social Science & Medicine, 239, 112532. https://doi.org/10.1016/j.socscimed.2019.112532
3. Singer, L. T., Linares, T. J., Ntiri, S., Henry, R., & Minnes, S. (2004). Psychosocial profiles of older adolescent MDMA users. Drug and Alcohol Dependence, 74(3), 245-252. https://doi.org/10.1016%2Fj.drugalcdep.2003.12.015
4. Koesters, S. C., Rogers, P. D., & Rajasingham, C. R. (2002). MDMA (‘ecstasy’) and other ‘club drugs’: The new epidemic. Pediatric Clinics, 49(2), 415-433. https://doi.org/10.1016/S0031-3955(01)00012-8
5. Jacobsen, L. K., Mencl, W. E., Pugh, K. R., Skudlarski, P., & Krystal, J. H. (2004). Preliminary evidence of hippocampal dysfunction in adolescent MDMA (“ecstasy”) users: possible relationship to neurotoxic effects. Psychopharmacology, 173, 383-390. https://doi.org/10.1007/s00213-003-1679-4
6. Bates, M. S., & Trujillo, K. A. (2021). Use and abuse of dissociative and psychedelic drugs in adolescence. Pharmacology Biochemistry and Behavior, 203, 173129. https://doi.org/10.1016/j.pbb.2021.173129
7. Morgan, C. J., Riccelli, M., Maitland, C. H., & Curran, H. V. (2004). Long-term effects of ketamine: evidence for a persisting impairment of source memory in recreational users. Drug and alcohol dependence, 75(3), 301-308. https://doi.org/10.1016/j.drugalcdep.2004.03.006
8. Bogadi, M., & Kaštelan, S. (2021). A potential effect of psilocybin on anxiety in neurotic personality structures in adolescents. Croatian Medical Journal, 62(5), 528-530. https://doi.org/10.3325/cmj.2021.62.528
9. Shah, K., Trivedi, C., Kamrai, D., Akbar, M., & Tankersley, W. (2022). Association of Psilocybin Use in Adolescents with Major Depressive Episode. European Psychiatry, 65(S1), S329-S329. https://doi.org/10.1192%2Fj.eurpsy.2022.837
10. Jones, G., Arias, D., & Nock, M. (2022). Associations between MDMA/ecstasy, classic psychedelics, and suicidal thoughts and behaviors in a sample of US adolescents. Scientific reports, 12(1), 21927. https://doi.org/10.1038/s41598-022-25658-5
Highlighted Institutes
These are the institutes, from companies to universities, who are working on Adolescence and Psychedelics.
Highlighted People
These are some of the best-known people, from researchers to entrepreneurs, working on Adolescence and Psychedelics.
Linked Research Papers & Trials
Pro & Business members will be able to see all linked papers and trials directly on this topic page.
This information is still available for you by selecting Adolescence and Psychedelics on the Papers and Trials pages respectively.
See the information directly on this page with a paid membership.

