This survey study (n=104) asked psychiatrists at two conferences about their knowledge (many aware of the promise) and opinions/concerns (lack of training, logistics, patients with contraindications) regarding psychedelic therapy. Those who worked more in research, know more about psychedelics, or were less concerned about the addictive potential scored higher in their beliefs on the effectiveness of psychedelic-assisted therapy.
Abstract
“Despite resurgent interest in psychedelic-assisted therapy, our insights into psychiatrists’ knowledge and opinions about medicinal psychedelic applications are surprisingly narrow. Therefore, we anonymously surveyed psychiatrists attending psychedelic didactic presentations at two national meetings about these issues using a 26-item questionnaire. Response rate was 40.20% (106/264). Respondents were 41.73 ± 13.31 years old (range: 24–80) and 64.42% were male. They largely believed psychedelics show treatment promise and strongly supported federal funding for medicinal psychedelic research. The most common concerns were the lack of trained psychedelic-assisted therapy providers, the logistics of psychedelic-assisted therapy delivery, the administration of psychedelics for patients with contraindications, and diversion. The most desired psychedelic-related educational topics were potential benefits of psychedelic-assisted therapy, how to conduct psychedelic-assisted therapy, psychedelic pharmacology, and psychedelic side effects. Factors associated with increased belief in psychedelics’ treatment potential included working primarily in research, scoring higher on a psychedelic knowledge test, and reporting less concern about psychedelics’ addictive potential. Working primarily in research and consult-liaison psychiatry fellowship training were positively associated with support for medicinal psychedelic legalization, while increased concerns about addictive potential and attending psychiatrist status were negatively associated. Support for legalization of non-medicinal psychedelic use was negatively associated with age and positively associated with support for legalization of medicinal psychedelic use.”
Authors: Brian S. Barnett, Yvan Beaussant, Franklin King 4th & Rick Doblin
Notes
Psychedelic-assisted therapy will need to be administrated not by dedicated researchers but by psychiatrists and other mental health care workers. A looming question for psychedelics as medicines can be paraphrased as “are medical professionals ready to administer psychedelics in the treatment of patients?” The promising clinical trials should be able to sway many, yet a stigma is still attached to psychedelics. The current paper adds more data to answer this question by surveying 104 psychiatrists over the course of two presentations about psychedelics at psychiatry conferences.
The survey asked psychiatrists first about their knowledge of psychedelics (e.g. if they knew which psychedelics were of natural origin & which clinical trials phase psilocybin studies are). They were then asked about their attitudes towards psychedelics, the questions also asked about what ways the psychiatrists would like to be informed or educate themselves on this topic.
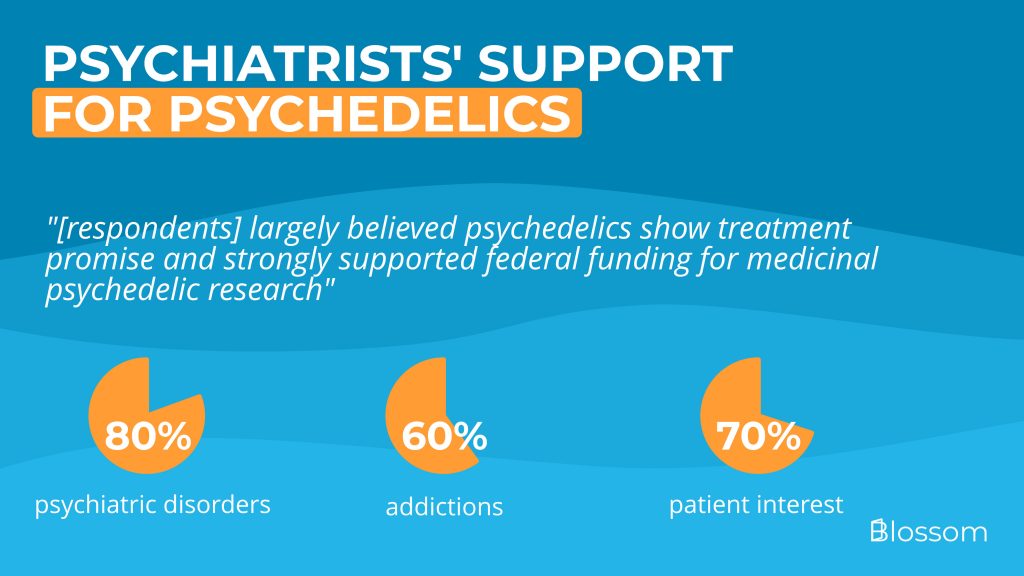
This is the support they found:
- 80% agreed that psychedelics show promise in treating psychiatric disorders, this was 60% for treating substance use disorders (e.g. alcoholism)
- 66% indicated concerns about a lack of trained psychedelic-assisted therapists, which matches nicely with them receiving less than two hours of psychedelic training
- 70% said that patients asked about psychedelic therapy a few times (60%) or often (10%)
This level of support is quite a bit higher than one would have expected only a few years ago. The study also found that nearly half of the participants knew that MDMA trials are in phase III. Even more surprising is that a third of attendees had read ‘How to Change Your Mind‘. But, what should keep into consideration is that the participants did self-select to attend a session about psychedelics, leading to a selection bias and possibly higher support than within the general population of psychiatrists.
One final observation was that some psychiatrists were concerned about the addictive potential of psychedelics. Those were also less likely to support them for substance use disorder treatments or legalization. The current evidence and a long history of recreational use find that the risk of addiction to psychedelics is (very) low. More education about the addictive potential, teaching the differentiation between psychedelics and a misguided conception of ‘drugs’ should play a part in the training psychiatrists receive.
The 26-item questionnaire given to psychiatrists is available here.
Summary
We anonymously surveyed psychiatrists attending psychedelic didactic presentations at two national meetings about their beliefs and opinions about medicinal psychedelic applications. Most believed psychedelics show treatment promise and strongly supported federal funding for medicinal psychedelic research.
Introduction
After decades of slow progress secondary to stigma, regulatory barriers, and limited research funding, medicinal psychedelic research has begun accelerating in recent years. Psilocybin, MDMA, and ayahuasca have shown promise in treating anxiety and depression, and treatment-resistant major depressive disorder.
Esketamine has been approved for treatment-resistant depression in the U.S., Canada, Europe, South Korea, and elsewhere, and promising findings suggest that legal opportunities exist for innovative psychiatrists to conduct effective psychedelic-assisted therapy.
Given the progress of psychedelic-assisted therapy on both clinical and investigational fronts, psychiatry should begin preparing for the likely arrival of psychedelic-assisted therapy in its current psychotherapy delivery model.
Psychedelic-assisted therapy presentations were attended by psychiatrists at two national psychiatric professional meetings in late 2019. They were surveyed to gain insights into their psychedelic knowledge and attitudes toward psychedelic-assisted therapies.
Survey design
The study instrument was an anonymous 26-item survey that asked participants about age, gender, training level, year of training completion, subspecialty fellowship training type, and primary daily work activity.
Data analysis
Data were managed using REDCap electronic data capture tools and statistically analyzed using Stata® version 12.0. Multivariate logistic analyses were used to investigate potential predictors of moderate or strong beliefs that psychedelics show promise in treating psychiatric and substance use disorders.
Results
The response rate was 40.20% (106/264), half were AAAP attendees, most were attending psychiatrists, 25.96% were residents, and 10.58% were fellows. Most worked in clinical care, with 7.69% working in research and 4.81% working in administration.
Most respondents believed psychedelics could treat psychiatric disorders and substance use disorders, and believed the federal government should fund medicinal psychedelic research. They also had concerns about the lack of trained psychedelic-assisted therapy providers and logistics of psychedelic-assisted therapy delivery.
Respondents reported receiving 1.53 – 1.76 hours of psychedelic didactics during residency training, though they believed psychedelics should receive 8.37 – 13.29 hours.
Multivariate logistic regression revealed that those working primarily in research held stronger positive beliefs about psychedelics’ treatment potential for psychiatric disorders, were more likely to support legalization of medicinal psychedelic use, and were less likely to be concerned about addictive potential.
Discussion
A self-selected group of psychiatrists attended a didactic session on psychedelics. They held favorable attitudes toward potential psychedelic psychiatric treatments, but had limited knowledge of where psychedelic-assisted therapy research currently stands.
Concerns raised by respondents about psychedelic-assisted therapy include a lack of trained providers, logistics and time demands of administering this treatment, and anticipated third-party reimbursement challenges. Non-physicians may play an important role in delivering this treatment.
Respondents expressed concern that psychedelic-assisted therapies might be administered to patients with contraindications, but were enthusiastic about improving their psychedelic knowledge. Some universities are now administering psychedelic-assisted therapy training programs, and MAPS has incorporated virtual training sessions into its program.
Psychiatry should collaborate with experts in psychology, social work, indigenous medicine, spiritual care, and other fields to develop low-cost training programs for psilocybin-assisted therapy.
Participants in our study wanted to learn more about psychedelic pharmacology, side effects, medication interactions, potential benefits of psychedelic-assisted therapy, and which patients to exclude from treatment.
Our findings contrast with those of a previous survey of psychiatrists on psychedelics, which found an association between favorable views of psychedelic treatment potential and younger age and male gender. We also found an association between increased age and less support for legalization of non-medicinal psychedelic use.
Concerns about psychedelics’ addictive potential were associated with decreased belief in psychedelics’ potential for treating substance use disorders and decreased support for legalization of medicinal psychedelic use. However, increased academic exposure to psychedelics might dispel inaccurate notions about them and improve support for psychedelic-assisted therapy among psychiatrists.
This study was limited by the self-selected nature of participants attending presentations on psychedelics, the moderate response rate, and the small sample size. It also may have been underpowered to detect some associations.
Future research should use larger, randomly selected national and international samples to study psychiatrists’ attitudes toward psychedelics and desired educational topics. This would help develop effective psychedelic educational offerings.
Authors
Authors associated with this publication with profiles on Blossom
Rick DoblinRick Doblin Ph.D. is the founder of MAPS. His persistent work since 1986 has been one of the main drivers behind why psychedelics (including MDMA) are now coming back to therapy.

