Key Insights
- A range of eating disorders exists. The most prevalent eating disorders are anorexia nervosa and bulimia nervosa, affecting roughly 16 million people across the globe. People with eating disorders experience a risk of increased mortality, high years lived with disability (YLD) rates and reduced quality of life.
- Using psychedelics to treat eating disorders is a relatively novel application of these substances. Clinical trials using psychedelics, including psilocybin and MDMA, to treat eating disorders are in the early stages at institutions such as Johns Hopkins and Imperial College London.
- A small number of companies are exploring this therapeutic application of psychedelics. Novamind and Tryp Therapeutics are two companies in this space, however, this number will likely increase as research progresses.
What are eating disorders?
Eating disorders are behavioural conditions characterized by severe and persistent disturbance in eating behaviours and associated distressing thoughts and emotions [1]. An array of eating disorders exist; anorexia nervosa, bulimia nervosa, binge eating disorder and pica, to name a few.
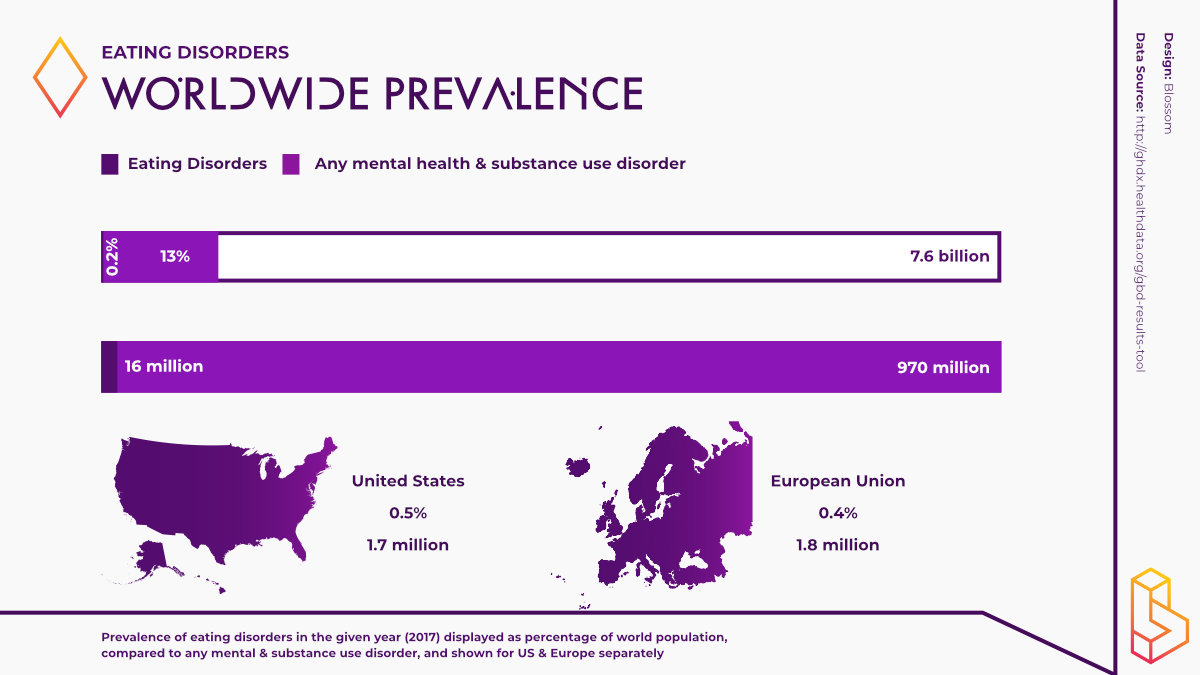
With an estimated 16 million people living with anorexia and bulimia, these disorders are the most common eating disorders across the globe [2]. Both anorexia and bulimia are more common in women however, eating disorders can occur at any age and affect any gender [1].
Despite treatment advances, mortality rates from disorders like anorexia and bulimia remain very high, yearly healthcare costs of patients with eating disorders are 48% higher than the general population and an estimated 3.3 million healthy life years are lost worldwide annually because of eating disorders [3].
Eating disorders are complex in nature. Thus, the exact causes of these disorders remain contentious, with interactions between biological, psychological and environmental factors thought to be involved [4].
Given the wide range of eating disorders, the symptoms underlying each disorder differ. According to the DSM-5, bulimia is characterized by recurrent episodes of binge-eating, recurrent inappropriate compensatory behaviours in order to prevent weight gain, such as self-induced vomiting, with these behaviours occurring at least once a week for 3 months [5].
With anorexia, patients restrict their energy intake relative to requirements, leading to significantly low body weight in the context of age, sex, developmental trajectory, and physical health, possess an intense fear of gaining weight and there is also a disturbance in the way these patients experience their body weight or shape [5].
Given the psychological nature of eating disorders, these disorders are commonly experienced comorbidly with disorders including major depressive disorder and anxiety disorders [6].
Conventional treatments
Treating eating disorders often involve a multidisciplinary team including; a mental health professional, a dietitian, a medical professional and a patients family members/loved ones. The conventional treatments for eating disorders often include a combination of psychotherapy, nutrition education, medical monitoring and sometimes medications [7].
Common forms of psychotherapy include cognitive-behavioural therapy (CBT), family-based therapy and group-based cognitive therapies.
Given the comorbidities associated with eating disorders, common medications used to treat these disorders include antidepressants, antipsychotics and mood stabilizers. In the case of anorexia, no medication has received FDA approval for the treatment of the disorder whereas in bulimia, the SSRI Fluoxetine, more commonly known as Prozac, is the most commonly utilized and the only FDA approved medication [8].
With these medications having limited success in treating eating disorders, research into the effectiveness of psychedelic drugs and the subsequent psychedelic-assisted psychotherapy treatment model, for treating these disorders is well underway.
Psychedelics and eating disorders
Research into the potential of psychedelics to treat eating disorders is a relatively novel phenomenon within the psychedelic community. Nevertheless, the potential of psychedelics to treat these disorders was not overlooked during the first era of psychedelic research.
The first known documented case of psilocybin being used to treat anorexia nervosa dates back to Paris, in 1959. This trial was recently revisited and translated to English in light of the recent renewed interest in using psychedelics to treat anorexia. In the trial, it was found that, after two separate injections of psilocybin, the patient stated she was able to understand the psychological cause of her illness.
Other psychedelics including ayahuasca, MDMA and ketamine, are also showing great promise in regard to alleviating the symptoms of various eating disorders.
In one study, individuals previously diagnosed with an eating disorder were interviewed regarding their experiences with conventional treatments for eating disorders and their experiences using ceremonial ayahuasca. Common themes amongst participants included a rapid reduction in thoughts and symptoms relating to their disorder, healing at the perceived root cause and greater self-love and self-acceptance, among others.
Led by the renowned Roland Griffiths, a research team at Johns Hopkins University is currently conducting a Phase I clinical trial into the safety and efficacy of psilocybin for treating persons with chronic anorexia. These researchers are hoping to determine if the positive changes observed in persons with anxiety and depression following the consumption of psilocybin in a supportive environment can be reproduced in those with anorexia.
To determine the effects directly related to anorexia, these researchers will utilize the Eating Disorder Quality of Life Scale (EDQLS), the Eating Disorder Examination Questionnaire (EDE-Q) and the Eating Disorder Examination (EDE) interview.
At the recent 2021 Horizons Conference in New York, Dr. Natalie Gukasyan from Johns Hopkins updated attendees on the progress of this trial. Surprisingly, the researchers found that patients had relatively mild psychological reactions to the already relatively high doses that were being administered. As result, researchers have increased the number of sessions to four as well as the maximum dose of psilocybin to 30mg.
Furthermore, the early results are showing that some participants have lower-than-expected subjective effects, more psychological support relative to other populations may be needed and that the therapeutic effects of psilocybin-assisted therapy take time.
In 2020, researchers made a case for using MDMA in the treatment of eating disorders. Now, another household name in the psychedelic community, MAPS, is testing this hypothesis and planning to conduct a Phase IIa trial exploring the potential of MDMA-assisted psychotherapy for the treatment of anorexia nervosa restricting-type, a subtype of the disorder as well as binge-eating disorder. Similar to those at Johns Hopkins, the researchers at MAPS are utilizing the EDE interview to determine effectiveness.
Researchers at Imperial College London are also exploring the effectiveness of psilocybin to treat anorexia in a current pilot study. Additionally, the secondary aim of this study is to use Magnetic Resonance Imaging (MRI) and Electroencephalography (EEG) to examine the neuronal underpinnings of treatment with psilocybin in this patient group.
Something which is often overlooked in drug development and medicine, in general, is the perspective of the people seeking treatment, such insights can be invaluable. A recent survey study (n=200) examined the views of people with eating disorders (EDs) with regard to psychedelic therapy. Over half of the respondents said they would take part in psychedelic research while 60% believed it is worthwhile continuing research in this area. Respondents also agreed that education regarding psychedelics and their use in psychiatry is needed.
How might psychedelics treat eating disorders?
As is the case with many mental disorders for which psychedelics hold promise, the exact mechanisms of action remain unknown. A growing body of research points to two pathways through which psychedelics might help individuals with eating disorders.
The first of these pathways relate to the default mode network (DMN) and the ability of psychedelics to alleviate symptoms related to serotonergic signalling in this region of the brain [9]. The DMN is a collection of pathways that govern our self-image, our autobiographical memories, and our deeply ingrained beliefs and thought patterns [10].
In those with eating disorders, overactivity in the DMN has been related to over caloric intake and food rules, compulsive exercise or eating behaviour patterns. Thus, by downplaying the signalling of neurotransmitters in this region, it helps to break eating disorder patterns that have become engrained in induvial and creates an opportunity to move beyond self-imposed limitations and start anew [9].
The second pathway involves the way in which psychedelics can help foster desirable brain states that might accelerate therapeutic processes. For example, MDMA improves mood and sociability, promoting the acceptance of and empathy for the self and others [11]. Thus, once consumed, MDMA allows persons to emotionally engage in psychotherapy without becoming overwhelmed with anxiety.
Psychedelic industry and eating disorders
A number of companies within the psychedelic space are focusing on harnessing the potential of psychedelics to treat eating disorders.
Headquartered in Toronto but mainly operating in Utah, Novamind is developing a network of clinics specializing in psychedelic medicines. At present, Novamind currently offers ketamine-assisted therapy for a range of mental disorders. Their Cedar Clinical Research branch is a contract research organization working toward utilizing psychedelics to treat eating disorders, amongst other disorders.
Reid Robison, CMO at Novamind, and Adele Lafrance have developed new therapies utilizing ketamine to treat eating disorders as well as other mental health disorders. Robinson and Lafrance are also working with MAPS, helping to lead their aforementioned study investigating MDMA-assisted therapy for eating disorders.
Additionally, Robinson and Lafrance have proposed three models of family-based psychedelic medicine in order to better the therapeutic outcomes for those with eating disorders [12]. Family-based therapies have often been cited as being extremely effective in helping those with eating disorders, especially in adolescents.
- The first model involves the recruitment of caregivers who learn specific skills to support their family member/loved one as they undergo psychedelic-assisted therapy.
- The second model proposes caregivers participate in the psychedelic therapy session alongside their loved one, thereby fostering a neurobiological bond to enhance the healing process.
- The third model involves caregivers who participate in psychedelic-assisted psychotherapy on behalf of their loved one, who, for medical or psychiatric reasons, cannot participate themselves. While this model may seem counterintuitive, psychedelic-assisted therapy can help caregivers gain a better understanding and fresh perspective on the condition of their loved one.
Tryp Therapeutics is another Canadian based company exploring the potential of psychedelics to treat eating disorders. Working with Dr Jennifer Miller at the University of Florida, Tryp and Dr Miller have begun designing a Phase IIa open-label clinical study utilizing TRP-8802, a synthetic derivative of psilocybin, in patients suffering from rare and orphan over-eating disorders.
In August this year, Tryp announced that the training of psychotherapists who will administer these drugs has been completed and the trial should commence in due process.
Given that there is an increasing amount of research regarding the effectiveness and safety of utilizing a range of psychedelics to treat depression and anxiety disorders, which are more often than not experienced comorbidly with eating disorders, research will continue into the potential of psychedelics for treating eating disorders.
References
1. American Psychiatric Association. (2021). Eating Disorders. Washington DC: American Psychiatric Association. Retrieved from https://www.psychiatry.org/patients-families/eating-disorders/what-are-eating-disorders
2. Dattani, S., Ritchie, H., & Roser, M. (2018). Mental Health. Our World in Data. https://ourworldindata.org/mental-health
3. Hoeken, D., & Hoek, H. (2020). Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Current Opinion in Psychiatry, 521-527. https://journals.lww.com/co-psychiatry/Fulltext/2020/11000/Review_of_the_burden_of_eating_disorders_.3.aspx
4. Muhlheim, L. (2020). Medications Used to Treat Eating Disorders. New York: Verywell Mind. Retrieved from https://www.verywellmind.com/medications-used-to-treat-eating-disorders-4153046
5. American Psychiatric Association. (2013). Eating Disorders – Diagnostic and statistical manual of mental disorders (5th ed.). Washington DC: American Psychiatric Association.
6. Pearlstein, T. (2002). Eating disorders and comorbidity. Archives of Women’s Mental Health, 67-78. https://link.springer.com/article/10.1007/s007370200002
7. Mayo Clinic. (2017). Eating disorder treatment: Know your options. Rochester: Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/eating-disorders/in-depth/eating-disorder-treatment/art-20046234
8. Muhlheim, L. (2020). Medications Used to Treat Eating Disorders. New York: Verywell Mind. Retrieved from https://www.verywellmind.com/medications-used-to-treat-eating-disorders-4153046
9. Lafrance, A., & Robinson, R. (2021). Psychedelics and Eating Disorders. Eating Disorder Resource Catalouge. https://www.edcatalogue.com/psychedelics-eating-disorders/
10. Buckner, R., Andrews-Hanna, J., & Schacter, D. (2008). The brain’s default network: anatomy, function, and relevance to disease. Annals of the New York Academy of Sciences, 1-38. Retrieved from https://pubmed.ncbi.nlm.nih.gov/18400922/
11. Hysek, C., Schmid, Y., Simmler, L., Domes, G., Preller, K., & Liechti, M. (2014). MDMA enhances emotional empathy and prosocial behavior. Social cognitive and affective neuroscience, 1645-52.
12. Lafrance, A., & Robinson, R. (2021). Psychedelics and Eating Disorders. Novamind. https://web.archive.org/web/20210309191105/https://novamind.ca/2021-01-29-psychedelics-and-eating-disorders/
Highlighted Institutes
These are the institutes, from companies to universities, who are working on Eating Disorders.
Novamind
Novamind has bold plans for building out a psychedelic ecosystem. One that spans from ketamine-assisted psychotherapy and psilocybin retreats to novel clinical trials.
Johns Hopkins University
Johns Hopkins University (Medicine) is host to the Center for Psychedelic and Consciousness Research, which is one of the leading research institutes into psychedelics. The center is led by Roland Griffiths and Matthew Johnson.
Tryp Therapeutics
Tryp Therapeutics is a clinical stage drug development company developing psilocybin products for various diseases/disorders including fibromyalgia.
Imperial College London
The Centre for Psychedelic Research studies the action (in the brain) and clinical use of psychedelics, with a focus on depression.
Highlighted People
These are some of the best-known people, from researchers to entrepreneurs, working on Eating Disorders.
Walter Kaye
Walter Kaye is the Director of the University of California, San Diego Eating Disorder Treatment and Research Program and is working with COMPASS Pathways on a trial with psilocybin.
Jennifer Miller
Dr Jennifer Miller is a Professor in the division of pediatric endocrinology at the University of Florida.
Adele Lafrance
Dr Adele Lafrance is a clinical psychologist, research scientist and published author.
Reid Robison
Reid Robison is CMO at Novamind.
Roland Griffiths
Roland R. Griffiths is one of the strongest voices in psychedelics research. With over 400 journal articles under his belt and as one of the first researchers in the psychedelics renaissance, he has been a vital part of the research community.
Linked Research Papers & Trials
Pro & Business members will be able to see all linked papers and trials directly on this topic page.
This information is still available for you by selecting Eating Disorders on the Papers and Trials pages respectively.
See the information directly on this page with a paid membership.

